
Can Someone With Diabetes Get A Pedicure: Discover 7 Comprehensive Tips
HOME | DIABETES EDUCATION | CAN SOMEONE WITH DIABETES GET A PEDICURE?
Before she does anything more with a client than shake her hand, Jill Tinetti carefully examines the health history section on her brand-new client card. Can someone with diabetes get a pedicure? With pedicure clients, she carefully evaluates the customer’s skin and nails and asks a few relatively casual concerns targeted at unearthing any signs or signs of diabetes.
As a registered nurse, Tinetti understands what to look for. And as a diabetic herself, she understands all too well what’s at stake. She is often asked the question, can someone with diabetes get a pedicure? Years earlier, long before she herself ended up being a certified nail tech; an unexpected nick incurred in the course of a pedicure landed her in the emergency room. Detected with cellulitis, she required 10 days of intravenous antibiotics to heal.
” I’m very cautious,” declares Tinetti, who’s worked at Tall Lawn Health Club in Evergreen, Colo., ever since getting her license 2 years ago. “with diabetic’s. I never nip their.”
With the growing popularity of pedicures and the increasing number of diabetics in the United States, nail techs increasingly are faced with the problem.
According to the Centers for Disease Control and Avoidance, more than 15.7 million Americans had diabetes in 1998. According to Douglas Albreski, D.P.M., a podiatrist who focuses on the skin disease and an assistant teacher at the University of Connecticut Health Center in Farmington, Conn., that number continues to increase at a fast pace in what specialists are calling a “diabetic epidemic.”
” Diabetes is a really serious illness,” includes Lee Sanders, D.P.M., the immediate previous president of health care and education for the American Diabetes Association (ADA) and chief of podiatry at the Veterans Administration Medical Center in Lebanon, Pa. “It’s become the leading cause of new cases for kidney failure, blindness, and nontraumatic amputation.”
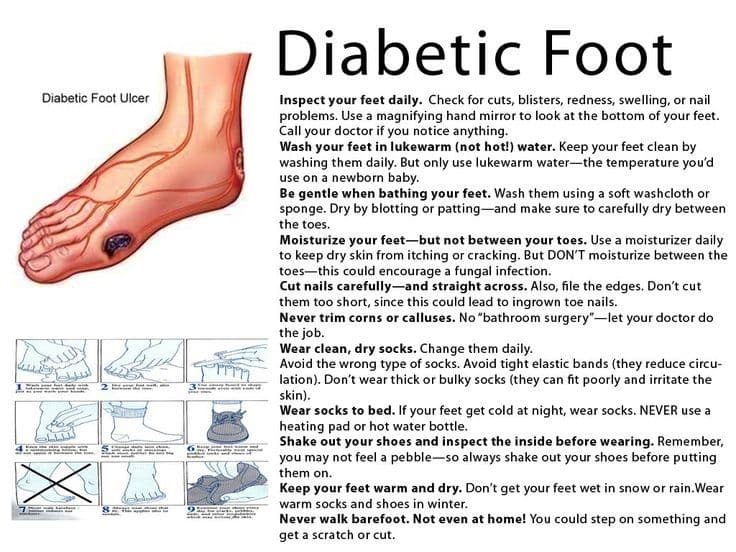
The Diabetic Foot: What You Should Know
Diabetes also is a leading cause of foot problems. Can someone with diabetes get a pedicure? Over time, every diabetic will experience some issues with his/her feet, says Dr. Sanders. And according to the ADA, 20% of diabetic healthcare facility admissions can be blamed on foot problems. Dr. Sanders has also asked the question, can someone with diabetes get a pedicure?
” Quite a few diabetics are diagnosed because they begin to experience foot issues,” Dr. Albreski observes, including that the three most severe foot problems for diabetics are neuropathy, bad blood circulation, and immune deficiencies.
Diabetic neuropathy (nerve damage straight associated with diabetes) incorporates a group of nerve diseases that can impact the feet in various methods. Damage to the motor nerve fibers deteriorates the muscles in the feet.
Poor blood circulation, or an inadequate circulation of blood, is another common issue for diabetics. With bad flow, it takes the body longer to heal itself and heightens the risk of infection. In diabetics with bad flow, even a small nick or an ingrown toenail can lead to severe health issues.
Says Dr. Albreski, diabetics are more susceptible to specific bacterial and fungal infections of the skin and nails. To the feet, diabetics are most likely to suffer dry, split skin, calluses, corns, and fungal infection of the nails (onychomycosis). Foot ulcers, especially over the ball of the foot or on the bottom of the huge toe, likewise prevail.

The Consultation: Can someone with diabetes get a pedicure?
Among the big concerns for nail techs has always been, should you or shouldn’t you do pedicures on diabetic customers? The standard reply has actually been to get an okay from the customer’s doctor. As Judi Shakula, D.P.M., of Grady Diabetes Center in Atlanta, points out, the theory does not work well in practice.
For one, the CDC approximates that approximately half of diabetics are as-yet-undiagnosed. Second, much of the customers who know they have the disease and are under a doctor’s care do not desire the trouble and may simply look for another pedicurist. Dr. Shakula thinks many medical professionals will err on the side of caution and automatically say no to prevent any liability in the event of an issue.
All diabetics posture a danger in the pedicure chair, emphasize the doctors we asked. Anybody with neuropathy, poor circulation, a present or previous foot ulcer, or amputation of all or any part of a foot (even if the feet appear healthy now, as they may with a diabetic who’s previously had an ulcer) is a high-risk diabetic and need to be declined.
Low-risk diabetics, on the other hand, have full feeling in their feet, great flow, and no signs of foot infections or defects, states Dr. Albreski. He and Dr. Shakula recommend assessing the condition of each client’s feet and asking some basic questions to assess the customer’s suitability for an expert pedicure.
First, try to find the following.
Thickened, yellow nails. These might suggest a fungal infection of the nails. A diabetic is twice as likely as the average individual to suffer from onychomycosis.
Any significant foot deformities. This includes hammertoes and bunions in addition to exceedingly built-up calluses and corns.
Thin, waxy-looking skin. This suggests bad blood circulation, which makes diabetics more prone to serious infections on their feet.
A purple, blue, or red shade. Pink is healthy; purple and blue suggest a circulatory problem; red signals a possible infection.
A “hot spot” or exceedingly cold feet. If one part of the foot feels warmer than the rest, that can suggest infection. Extreme cold, on the other hand, points to poor circulation. “At the start of the upper part of the leg to the very bottom of the feet the temperature level needs to remain consistent,” Dr. Albreski describes. “We call it the ‘gradient impact.'”.
A loss of feeling. Evaluate the feeling in your client’s foot by asking her to look away while you gently brush the top of her foot with a tissue.
Exists hair on the toes? While it might not, please the eyes, hair on the toes is a positive (though unscientific) indication of excellent blood circulation.
As you make these basic observations, ask your brand-new customer these concerns:.
- Has your doctor ever stated you have bad circulation?
- Can someone with diabetes get a pedicure
- Do you experience any tingling or burning in your feet?
- Do you smoke? (Cigarette smokers tend to have poor circulation, and diabetics who smoke are particularly at danger for circulatory and neuropathic disorders.)
- Do you have any loss of sensation in your feet?
- Have you ever had a foot ulcer?
- How well is your blood sugar level managed? (Well-controlled blood sugar has actually been revealed to slow illness progression. Badly controlled blood glucose increases the possibility of more severe issues that appear faster.)
- When’s the last time your physician analyzed your feet? What were his observations? (Diabetics must have their feet analyzed by a physician a minimum of when a year, more often if they have problems.)
- A favorable answer to any of the very first five concerns is, naturally, a negative for proceeding with the service.
Can Someone With Diabetes Get A Pedicure: Step-by-Step.
Even with low-risk diabetics, you need to exercise severe care in taking care of their feet. With the help of Drs. Albreski, Sanders, and Shakula, NAILS developed the following pedicure strategy specifically for use with diabetic customers.
Prior to you even start the service they emphasize the need for tidy workstations, towels, and hands, sterilized implements, and fresh non reusable materials (such as files and orangewood sticks) for all clients, but especially diabetics. “Have a healthy regard for the possible issues and know how to prevent them,” Dr. Sanders worries.
They advise against utilizing chemical or mechanical exfoliants on the feet– which include razors or blades, pumice stones, foot files, or exfoliants such as glycolic acid or sea salt scrubs. Any of these tools carry the danger of breaking or otherwise hurting the skin– a risk too great to take with a diabetic. If you have a customer with diabetes who needs a callus or corn reduced, cuticles trimmed, or an ingrown nail treated, refer her instantly to a foot care expert such as a podiatrist.
Now, on with the service.
Action 1: Carefully wash her feet with an antibacterial soap and tepid water then pat dry.
Explanation: All 3 podiatrists suggest against foot soaks, even in tepid water. While the main concern is that a diabetic is more easily burned because of the loss of feeling, Dr. Sanders worries that soaking in water may worsen the dry skin so typical to diabetics.
” We’re also concerned now about cross-contamination,” notes Dr. Albreski. “The fungus that trigger skin infections are all over, and while the majority of people may not pick it up from a contaminated whirlpool, the diabetic simply might due to the fact that her body immune system isn’t as strong.”.
Step 2: Trim and shape the nails as preferred, being specifically careful not to nip the skin.
Explanation: A lot of diabetics are advised to submit down their toenails to the desired length, however Dr. Shakula says pedicurists can cut them with care if the nails are not misshapen or excessively thickened.
” Do not dig under the nail plate or gauge at the corners,” she recommends. “And never ever utilize a drill on the feet.”.
Action 3: Use a moderate cuticle treatment to soften cuticles. Do not, however, trim or push back the cuticles, cautions Dr. Albreski.
Explanation: “The cuticle works as a protective structure to keep germs and fungus from getting under the nail fold,” Dr. Sanders notes. Keep in mind, diabetics are more vulnerable to bacterial and fungal infections of the skin and nail. Can someone with diabetes get a pedicure, when present, these kinds of infections take longer to heal and are more likely to spread out and trigger a severe health problem.
Step 4: Next, use a hydrating lotion to the tops and bottoms of the feet– but prevent the areas in between the toes.
Description. Poor circulation can also cause issues with healing. Usually, the body keeps a steady supply of fresh blood flowing to heal broken tissues. Poor flow means a bad flow of blood, which slows healing.
Even a small cut or ingrown nail might take a long period of time to recover, which increases the likelihood of an infection. However, the areas in between the toes generally trap wetness, no matter how dry the rest of the foot is. Applying a cream or lotion in between the toes just traps more wetness and might cause the skin to break down, which in turn invites infection.
When it comes to what type of lotion to utilize, Dr. Albreski and Dr. Sanders suggest creams consisting of lactic acid or 10% urea. Dr Shakula, on the other hand, thinks pedicurists can utilize most moderate exfoliating creams. She concurs that moisturizers containing lactic acid are most efficient at softening the tough, dry skin so typical to diabetic feet.
Step 5: Massage each foot carefully however completely, rubbing toward the heart.
Description: A favorite with the majority of customers, diabetics can gain from massage because it improves flow, albeit temporarily.
Step 6: Polish the nails as wanted.
While a month-to-month pedicure suffices to preserve foot health for a lot of clients, diabetics need everyday foot care. However, as Dr. Albreski keeps in mind, “Most diabetics are aware of the need and they’ll inform you they’re on top of it, however they do not rather follow through in practice.”.
Advise these customers to carefully clean and visually examine their feet for injuries each day. Recommend them to finish their self-inspection with a liberal slathering of moisturizing lotion on the tops and bottoms of the feet to assist heal and prevent dry skin.
If, after all these preventative measures, you mistakenly nick or cut a diabetic client, Dr. Albreski urges you to confess the error and do something about it to avoid the injury from ending up being severe. “It’s not malpractice or malfunctioning workmanship to nick somebody,” he states. “What will get you into trouble is not attending to the scenario correctly.”
Citing 2 lawsuits he understands versus pedicurists, Dr. Albreski emphasizes the requirement for honesty and professionalism with clients. The question that will come up is, can someone with diabetes get a pedicure?
He recommends instantly stopping the service and performing standard first aid care: Utilize a styptic pencil to stop any bleeding, apply a triple antibiotic cream such as Neosporin, then gently bandage the website. Discuss to the customer what you did to treat the wound, then suggest that she notify her primary care physician of the injury and seek his opinion on whether she needs a physician’s care.
” Jot down whatever you did and said to the client and keep it in a file in case anybody returns to you later on,” Dr. Albreski states. You may even think about establishing a mishap or injury report comparable to those utilized by some child care centers. In this case, you might quickly note the injury, how it was treated in the beauty parlor, and repeat in writing the suggestion that the client seek her primary care physician’s recommendations on more treatment of the injury.
Choose your platform, share this story!
Facebook Twitter LinkedIn Pinterest



